Sengkang General Hospital will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg
“I’m a urologist who got prostate cancer”
“I’M A UROLOGIST WHO GOT PROSTATE CANCER.
THIS IS WHAT I’VE LEARNT.”
Many of us often ignore symptoms, deeming ourselves too busy to go for a checkup, or we self-medicate — until it’s too late. This can happen to anyone, even if you’re a seasoned urologist with 37 years of medical experience.
Most of us don’t pay enough attention to our health. We tend to delay seeing the doctor, brush off symptoms and carry on with our busy lives thinking it is not serious — even if the warning signs are there.
That was what the former CEO of SKH, Professor Christopher Cheng, believed too, until he was diagnosed with cancer. As an experienced urologist, Prof Cheng has devoted his life to preventing and curing cancers, especially prostate cancer. He thought he knew all about prostate cancer and what patients go through until in 2017 — in an ironic twist of fate — he experienced the condition himself as a patient.

You started experiencing symptoms early but delayed getting checked. In hindsight, what could you have done differently?
Prof Cheng: Over the years, I developed symptoms, one of which was urine retention which meant I was unable to empty out my bladder. I’d been delaying having my conditions checked because there was simply no time for me to do so amidst all my responsibilities as the chief executive of a new hospital then. By the time I finally got myself checked, my symptoms were worse than many of my patients.
As it turned out, it was cancer that caused some of my symptoms. Despite thinking my cancer risk was small, subsequent medical examinations had suggested that the cancer may not be curable. In hindsight, I should have seen someone and got myself treated earlier. I was hoping it wasn’t an emergency as I could tolerate the symptoms, and that was foolish.
Describe your experience when roles were reversed and you became the patient.
Prof Cheng: I was in an unusual situation as I’m a urologist, specialising in prostate cancer. My juniors were looking after their boss who probably knew a thing or two more than them. I wanted to be a ‘model patient’
but I was frightened and fearful and my anxiety was real. As a patient, I learned that fear cannot be dismissed simply by using common words to comfort — a patient will never ever be really assured. A patient’s fear is genuine, and medical professionals (like me) can sometimes come across as dismissive and not take their patient’s fear with an open heart.
What memorable experiences did you have with the team who looked after you?
Prof Cheng: I’ve encountered many angels in my journey. Everyone showed professionalism, concern and care. But there was a particular nurse who really touched me as a patient. The difference was in the way she encouraged me with a sense of caring urgency whenever she made her rounds. She even swapped shifts to make sure she was there on the first night I was warded after surgery. It showed me that it’s the person and the humanity that really makes the difference, and that she simply wasn’t just going through the motions.
On that note, how do you think medical practitioners can find that balance between having the technical know-how and being an empathic person?
Prof Cheng: In my experience as a patient, I realise medical practitioners sometimes unwittingly put people through a lot of basic yet stressful or painful routines. There were incidences during my own journey that have made me more mindful and conscious of how we treat patients. I hope medical professionals realise this, and that patients need compassion and understanding. Having the expertise is a given. It’s not about how many certificates or awards you have on the wall—what’s more critical is having empathy and connecting with patients at the heart level, not superficial level.
Having gone through the same experience as your patients, what would be your most important advice?
Prof Cheng: Many—men in particular—are perpetually in denial, partly because of our social upbringing and environment. We are expected to ‘be a man’ and bear with the pain and inconvenience. Perhaps this makes us believe we are indispensable or irreplaceable, and that ‘work is more important than health’ to provide for our family.
If you’re in denial but know you have a problem, go to an expert to get it fixed, rather than selfmedicate. I see this tendency to ignore symptoms in patients all the time. So yes, don’t try to be a ‘hero’, you have to look after yourself before you can look after others.
Just like in the current pandemic, getting the vaccine would be the best way if you want to look after and protect your family and fellow citizens. Seize the opportunity to get vaccinated now while our community cases are still low.

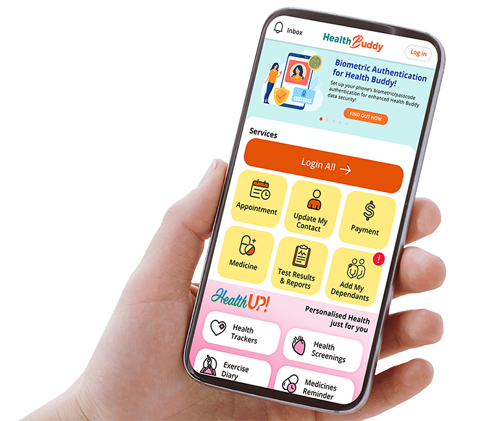
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.