Introduction
Swallowing
Difficulty in swallowing liquids and/or solids.
Language
Difficulty in reading, writing, comprehension and use of language.
Speech
Difficulty in the clear production of speech sounds as a result of muscle weakness and/or a motor coordination deficit
Voice
Difficulty in the appropriate use of voice quality, volume and pitch to communicate effectively with others.
Fluency
Difficulty in the flow of speech in the form of repetitions, prolongations and/or blocks, also known as stuttering.
Hearing Impairment
Difficulty in communication arising from a hearing loss.
What is dysphagia?
Dysphagia is a difficulty in swallowing liquids and/or solids, which may result in liquids or solids entering the airway and into the lungs. This is common in people with stroke, neurodegenerative diseases (e.g. dementia), respiratory disorder, and head and neck cancers. When left unmanaged, this may lead to chest infections (aspiration pneumonia) which can be life-threatening.
Swallowing Assessment
During an assessment, the Speech Therapist may:
- Obtain a case history to understand your swallowing difficulty and medical conditions that can contribute to this
- Assess and evaluate the strength and movement of muscles involved in swallowing
- Assess and evaluate the safety of swallowing during eating and drinking
If necessary, instrumental assessments like the Videofluoroscopic Swallow Study (VFSS) or Flexible Endoscopic Evaluation of Swallowing (FEES) may also be available for patients requiring these services.
Swallowing Therapy*
During therapy, the Speech Therapist may:
- Prescribe and review appropriate exercises taught to patients to improve the function of your swallow muscles
- If suitable, relevant biofeedback devices may also be used in conjunction with swallowing exercises taught to supplement therapy
Instrumental Swallowing Assessments*
Videofluoroscopic Swallowing Study (VFSS)
VFSS is an instrumental swallowing assessment done under X-Ray to assess the patient’s swallowing function across a variety of foods and liquids objectively. This is conducted by the Speech Therapist, the radiologist and the radiographer. Based on the findings, the appropriate diet and fluids may be recommended, together with the associated swallowing rehabilitation exercises prescribed to optimise the swallowing function.
Flexible Endoscopic Evaluation of Swallowing (FEES)
FEES is a procedure in which a thin, flexible endoscope is passed through the nose by the Speech Therapist to assess the swallowing function of the patient objectively. During the procedure, the patient may be required to eat and drink various food and fluids of different consistencies coloured with food dye. Based on the findings, the appropriate diet and fluids may be recommended, together with the associated swallowing rehabilitation exercises prescribed to optimise the swallowing function.
Speech and Swallow Airway (SSA) Clinic*
As part of a multidisciplinary team comprising doctors and allied health professionals, the Speech Therapist helps to oversee and manage the swallowing and communication issues that may arise after a tracheostomy. A tracheostomy is a medical procedure done by the surgeon for patients who may need added support to facilitate breathing and tracheal hygiene. This is done by creating an opening at the neck that connects to the airway via a tracheostomy tube. If suitable, the clinical information obtained in the process may also help patients wean off the tube completely.
Nutrition and Swallow Clinic*
- Are currently on transitioning feeding (e.g. tube to oral feeding)
- Requires supplements (e.g. Ensure milk supplements)
- Are transitioning between diets (e.g. completely blended to minced diet)
- May display poor oral intake
Device Related Rehabilitation (DRR) Clinic*
Our team of Speech Therapists in DRR Clinic specialises in the teaching of rehabilitation exercises using assistive devices for patients with swallowing difficulties from pre-existing medical conditions. Example of assistive devices include:
- Surface Electromyography (sEMG) device - it provides visual feedback of a patient’s muscle function, allowing them to self-monitor their performance during swallowing exercises. This enhances the efficacy of prescribed swallowing exercises.
- Iowa Oral Performance Instrument (IoPI) - it objectively measures the lip and tongue strength via resistance training, providing feedback on patients’ performance during oral motor exercise programs.
What is aphasia?
Aphasia is an acquired communication disorder that results in difficulties in understanding and using language. This may include difficulties in reading comprehension, understanding what others are saying to you, speaking and writing. Aphasia is commonly experienced by people who has been diagnosed with a neurological disorder such as stroke, an acquired traumatic brain injury or brain tumor.
What is dysarthria?
Dysarthria is a speech disorder often caused by muscle weakness. Some characteristics of dysarthria may include slurred or unclear speech, reduced speaking volume, increased or slowed speaking rate. Dysarthria is commonly seen in people with stroke and neurodegenerative diseases such as Parkinson’s Disease.
What is apraxia?
Apraxia of speech is a speech disorder caused by difficulty coordinating the muscles used for speech such as the tongue and lips in the right way to produce sounds and/or words for speech. In some cases, patients might not be able to speak at all. Apraxia is often experienced by people who has been diagnosed with stroke and/or an acquired traumatic brain injury.
What is cognitive-communication disorder?
Acquired cognitive communication deficits are changes to reasoning, attention, memory, organisation or planning, insight and/or social communication skills that may often result in difficulties with communicating with others in the community. This may occur after a stroke, tumour, brain injury, progressive degenerative brain disorders or other neurological damage.
Communication Clinic
Communication Assessment
During an assessment, our speech therapists will:
- Obtain a case history to understand your communication difficulties and its impact on your activities of daily living.
- Assess your communication difficulties with various tools and assessments. We also provide formal assessment reports on request.
- Assess and discuss your communication goals and needs for therapy.
Communication Therapy
For therapy, our speech therapists will:
- Provide individualised therapy tailored towards your goals and needs (e.g. return to work goals).
- Provide communication strategies and techniques for cares
- Provide alternative and augmentative forms of communication such as a picture communication board (i.e. AAC) for suitable candidates.
We can provide therapy in English, Mandarin and dialects such as Cantonese, Teochew and Hokkien.
Paediatric Speech and Language Clinic
Our Paediatric Speech Therapy Team specialises in the assessment and management of communication difficulties for the paediatric population (children aged 1 - 18 years old).
We assess, diagnose and treat children and adolescents with disorders or difficulties related to speaking, understanding and using language effectively. This may include:
- Speech sound disorders - distortion and/or mispronunciation of sounds produced
- Developmental language delays or disorders - difficulty understanding others, and/or expressing him or herself at an age- appropriate level.
- Fluency disorders – also known as stuttering, where there are difficulties in the flow of speech.
- Social communication disorders – difficulties using verbal and non-verbal communication appropriately in social situations.
What is a speech sound disorder (SSD)?
- It is common for young children learning to speak to make mistakes in their speech sounds during the first few years of speech development.
- However, it is not expected as a child gets older. SSD occurs when these mistakes persist past a certain age.
- SSD is a collective term, with several subcategories that include articulation disorder, phonological disorder and childhood apraxia of speech.
What is a developmental language disorder (DLD)?
- DLD is a condition that affects children’s ability to learn language skills.
- The child may have problems following directions, understanding questions, learning new words and/or saying sentences.
- DLD occurs in approximately 7 to 8% of preschool children and is more likely to affect boys than girls.
What is a social communication disorder (SCD)?
- Difficulties with the use of verbal and non-verbal language for social purposes.
- These include communicating in an appropriate manner for the particular social context, following rules for conversation, and understanding implicit nuances in language for social communication.
Paediatric Speech and Language Assessment
During an assessment, our speech therapists will:
- Assess and diagnose your child’s difficulties
- Determine the need for therapy
Paediatric Speech and Language Therapy
For therapy, our speech therapists will:
- Prepare a specific plan and set goals for your child
- Administer therapy to help your child communicate better
- Teach you activities and give suggestions to help your child practice at home
Voice
What is a voice disorder?
A voice disorder occurs when voice quality, pitch and/or loudness are impaired and prevent the speaker from communicating with others effectively.
We address voice disorders related to:
- Occupational voice demands
- Age-related voice changes
- Laryngitis
- Vocal nodules, polyps or cysts
- Vocal fold paralysis or paresis tremor
- Spasmodic dysphonia
- Chronic cough
- Laryngeal dysfunction
We also provide gender-affirming voice and communication training for transgender individuals.
Voice Assessment
During an assessment, our speech therapists will:
- Obtain a detailed case history concerning the voice problem you are seeking help for
- Ask questions to understand the nature and extent of your voice use in daily life
- Listen to your voice through various tasks to evaluate your voice quality, pitch and loudness
In addition, we partner with doctors in Ear, Nose and Throat (ENT) to conduct a specialist voice clinic. In this clinic, patients are seen jointly by a voice-specialised ENT surgeon and speech therapist. We provide consultation, videostroboscopic examination of the larynx (using a flexible scope with strobe lighting to take clear, detailed images of the voice box), and advanced diagnosis of all voice problems. Together with patients, we will develop a plan of care that may involve a combination of medical, surgical and/or therapeutic treatment.
Voice Therapy
If therapy is recommended, our speech therapists will:
- Design a treatment plan to reduce hoarseness and improve your voice condition
- Guide you towards healthy vocal and lifestyle behaviours to assist in vocal fold recovery
- Prescribe voice techniques and exercises to rehabilitate and optimise your voice quality
Voice therapy is the first line of treatment for many voice conditions and can be highly effective in treating hoarseness in patients of all ages. Generally, voice therapy consists of one therapy session each week for 4-8 weeks. The duration of therapy depends on the severity of hoarseness, nature of the underlying voice disorder, co-occurring medical treatment, and patient commitment to the treatment outside therapy sessions. With close adherence to therapy, patients are often able to restore their voices and meet their daily speaking needs successfully.
Fluency Therapy
Our Fluency Clinic provides assessment and treatment to individuals across all ages for the assessment and treatment of stuttering.
Fluency Assessment
- Ask questions to understand how stuttering presents in your speech and daily life
- Listen to your speech and evaluate any stuttering behaviours
- Determine the severity of stuttering
- Explain the nature and cause of stuttering
- Discuss your goals for treatment and the best options available
Fluency Treatment
- The Lidcombe Program
- The Westmead Program
- The Oakville Program
- Self-Imposed Time-Out
- Smooth Speech Technique
Hearing impairment
What is aural rehabilitation?
Aural rehabilitation is the assessment and management of hearing loss and its impact on communication.
Aural Rehabilitation Clinic*
Aural Rehabilitation (AR) is often used as an integral component in the overall management of individuals with hearing loss by a team of Audiologists, ENTs and Speech Language Therapists.
Aural rehabilitation is conducted by our Speech Therapists, with the aim of reducing the impact of hearing loss on our patients’ communication and quality of life. For individuals who have undergone a cochlear implantation, rehabilitation includes auditory training, speech therapy, training on communication repair strategies and telephone training.
Additional Services
Community-Based Therapy Services
In addition to the outpatient clinical services provided at Sengkang General Hospital (SKH), our Speech Therapists are actively involved in multiple projects in the wider community of the Northeast region. They include:
- The H2H Programme - a transitional hospital to home care programme to ensure smooth transition of care for patients who are bedbound, and/or may have difficulties attending outpatient follow up appointments.
- Project ASPIRE - a community care clinical service to manage frailty among seniors living in the community, in which participants will receive medical, nursing, physiotherapy, occupational therapy, speech therapy and dietetics services as needed. It is a collaboration with St Luke’s Eldercare (SLEC), SATA CommHealth, selected Senior Activity Centres (SACs) in the Northeast, and AIC’s Community Network for Seniors (CNS).
- Speech Therapy services to Nursing Homes - we support our community nursing homes by providing routine reviews to residents with swallowing difficulties and provide education to nursing staff as needed.
- Talks and workshops for family, caregivers, and professional colleagues in care facilities (such as schools, eldercare centres, and Singhealth Polyclinics) to raise awareness of swallowing and communication disorders and the role of speech therapy, and to support them in caring for loved ones and patients who have these disorders and their loved ones.
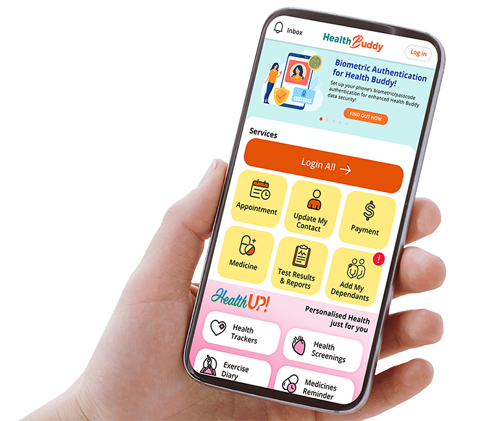
Video-Consultation Services
In addition to in-clinic consultation services, our Speech Therapists offer speech therapy via online video consultation. Our therapists will be able to interact with patients, perform diagnostic assessments, and provide intervention in real-time during remote sessions. Our video-consultation sessions are largely similar to face-to-face consultation with some modification of therapy methods and materials to better suit the online environment.
Patients managed via video-consultation will require a personal computer, tablet or smartphone with a webcam and internet connection. Speak with your Speech Therapist to find out whether receiving therapy via video-consultation may be suitable for you.
FAQs
1. How can I obtain an outpatient appointment to see a speech therapist?
A referral letter to Sengkang General Hospital’s speech therapy department is needed. You may obtain a referral from any SMC-registered doctor for SKH Speech Therapy services. Consultation charges will vary depending on referral source.
2. What can I expect in a speech therapy session?
Our Speech Therapists will assess and evaluate your communication and/or swallowing difficulties and prescribe the appropriate interventions for you. We may speak to your family members to have a better understanding of your difficulties.
3. How long will the treatment progress take?
An initial speech therapy assessment session will usually run for 45 to 60 minutes. A typical therapy session will last approximately 30 to 60 minutes, depending on the nature of your concern (e.g. swallowing or communication concerns).
Your speech therapist will discuss the frequency of therapy that is suitable for you, depending on your needs and progress.
4. Do you conduct therapy in other languages?
Yes, we currently offer speech therapy sessions in English and Mandarin. We may also require the presence of a caregiver to assist in translation for your loved ones during the sessions.
Contact Us
You may contact us at speechtherapy@skh.com.sg for any queries. To make any changes to your existing appointment, please call 6930 6000. Alternatively, you can fill up this form:
Location
We are located at Sengkang General Hospital, Outpatient Rehabilitation Centre, Blk 8, Level 2 (via Lobby C).
News