Sengkang General Hospital will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg
Is My Liver Fat?
A ‘silent’ disease, non-alcoholic fatty liver disease could be affecting you, even if you have no symptoms. Find out more.
“Fatty liver?” A 52-year-old patient expressed surprise with this diagnosis after a routine ultrasound scan for an unrelated condition. The diagnosis seemed improbable – he leads an active lifestyle, walks two kilometres to work daily, and maintains a healthy BMI of 25. Though deskbound, he neither smokes nor drinks alcohol, and has no major health conditions. In fact, he appeared to be the picture of health.
In Singapore, his profile would match many adults aged over 40, but what this patient has is Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD), which occurs when excessive fat builds up in the liver, unrelated to alcohol consumption.
This disease, previously known as Non-Alcoholic Fatty Liver Disease (NAFLD), was renamed MASLD recently to emphasise the association with metabolic dysfunction that causes the condition.
Local studies reveal a concerning trend: Among patients undergoing gall bladder removal, fatty liver cases rose significantly from 40% (2001 to 2004) to 56.6% (2011 to 2014). The prevalence is expected to increase over time.
What is MASLD?
“MASLD is caused by a metabolic syndrome that includes obesity, diabetes, high cholesterol, and high blood pressure,” explains Dr Li Huanghuan, Associate Consultant, Gastroenterology and Hepatology Service, Sengkang General Hospital.
Due to sedentary lifestyles and lack of exercise, and with many eating more processed and high-calorie foods, there is a high chance many Singaporeans are obese and have type 2 diabetes, high cholesterol, and high blood pressure – regardless of hereditary factors.
Dr Li shares, “People over 40 are at increased risk of developing MASLD as they’re also at risk of metabolic syndrome, even if they don’t drink or smoke.” MASLD develops when these metabolic factors are left unchecked:
- Being obese with excess body fat, especially visceral fat around the stomach
- Insulin resistance in type 2 diabetes
- Poorly controlled high cholesterol and blood pressure
Less common causes of fatty liver include long-term use of certain medications like corticosteroids, tamoxifen, methotrexate, and antiviral drugs. In addition, medical conditions such as polycystic ovary syndrome (PCOS), hypothyroidism, and obstructive sleep apnoea can also contribute.
“It is important to note that these factors often interact and compound each other, accelerating fatty liver development,” advises Dr Li.
A ‘Silent’ Disease
MASLD often goes undetected as it shows no symptoms in its early stages. Most people discover they have it during routine health check-ups or while being tested for other conditions, as seen in our patient’s story.
Diagnosing MASLD begins with a liver function test, followed by an ultrasound scan. Doctors then use the FIB-4 test, a non-invasive scoring system based on age, liver function test results and platelet count to assess how severe the liver fibrosis (thickening and scarring of connective tissue) is.
Dr Li explains, “It's a simple and cost-effective tool that can help identify patients who may need further evaluation or have a higher risk of advanced fibrosis.”
If the FIB-4 results are abnormal, more investigations will follow. The last option is liver biopsy. “Although it’s the gold standard for diagnosis, liver biopsy is more invasive and typically reserved for only cases where other tests are inconclusive,” cautions Dr Li.
Managing MASLD
The good news is that it is possible to control MASLD! This involves lifestyle modifications with weight loss (depending on the patient’s weight), regular exercise, and diet changes, and avoiding alcohol.
“Tight control of metabolic syndrome conditions like diabetes, high blood pressure, and high cholesterol is a must”, Dr Li stressed. Besides lifestyle modifications, vitamin E has been shown arguably to improve liver enzymes in MASLD but not liver fibrosis. There are also new medications, such as semaglutide, that shows promise in treating diabetes and obesity. Recent studies have shown that semaglutide can reduce liver fat and inflammation.
Diet and exercise can prevent MASLD or manage it at the early stage. “Aim for at least 150 minutes of moderate-intensity exercise weekly – activities like brisk walking, cycling, and swimming, where you can maintain a conversation while your heart rate is at 50-70% of maximum activity,” advises Dr Li.
Follow a Mediterranean-style diet rich in fruits, vegetables, whole grains, and lean proteins, with healthy fats like olive oil and nuts. Avoid high-calorie diets high in saturated fats and simple sugars, and limit red meat and processed foods. Reduce intake of sugary drinks – and here’s good news: moderate consumption of coffee has potentially been linked to reduced liver fat!

Fight These Common MASLD Myths
Many people believe they are safe from MASLD if they are generally well or feel healthy. Here are the facts!
Myth 1: MASLD only affects those who are overweight
Fact: While MASLD typically affects overweight people, 10-20% of patients have ‘lean MASLD’ – occurring in people of normal weight due to factors like family history or the body’s difficulty in processing sugar, even when they appear healthy.
Myth 2: MASLD is not serious
Fact: If not managed well, MASLD can lead to cirrhosis, liver failure and liver cancer. It is a leading cause of liver transplants in the world.
Myth 3: MASLD is rare in young people
Fact: Cases are rising in younger age groups due to childhood obesity, sedentary lifestyles, poor diets, and genetic factors.
Myth 4: MASLD can’t be reversed
Fact: In its early stages, MASLD can improve and even be reversed with appropriate lifestyle changes. Advanced stages can be stabilised but not reversed.
Myth 5: MASLD can be cured with supplements
Fact: Most ‘liver supplements’ lack clinical evidence and are not a substitute for lifestyle changes and proper medical care.
Myth 6: MASLD is always caused by a poor diet
Fact: Diet does play a role, but other factors like genetics, medications, and other related conditions also contribute.
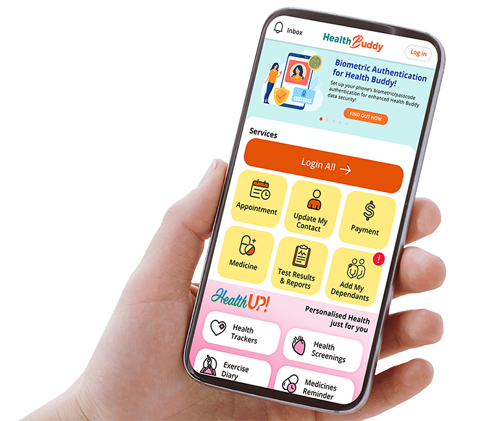
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.