Make No Bones About Osteoporosis
Osteoporosis is often called the silent killer as there are no signs or symptoms until a fracture happens. Contrary to popular belief, bone health is important to everyone at every age, not just for seniors. Here's what you need to know.
Why is osteoporosis serious?
"Up to 50% of patients with fractures didn't know they had osteoporosis prior to suffering an injury or fracture," shares Dr Donovan Tay, Senior Consultant in Endocrinology, Department of General Medicine at SKH.
Osteoporosis happens when your bones become brittle, lose strength and break easily. Undiagnosed and untreated, it is a silent disease that can lead to serious health problems, affect mobility and quality of life.
It is estimated that an osteoporosis-related fracture happens every three seconds worldwide. In Singapore, hip fracture admissions have also gone up to 2,729 cases in 2020 from 1,487 in 2017, due to the higher proportion of elderly people. With this number projected to hit 9,000 by 2050, osteoporosis is fast become a major health concern.
Who are at risk?
The older a person is, the higher the risk of developing osteoporosis. Post-menopausal women over the age of 65 and men above 70 are more likely to develop osteoporosis.
While certain people are more at risk, some risk factors such as gender, age, race, family history, or body frame size are fixed and cannot be changed. However, Dr Tay says risk factors like smoking, excessive alcohol, lack of exercise, and having a diet low in calcium or vitamin D are within your control.
Why is osteoporosis more common in women?
Women tend to have smaller, thinner bones than men. Women also undergo menopause where their estrogen levels drop. Estrogen protects the bone and the decrease in estrogen results in bone loss. About 2% of bone is lost per year after menopause.
What are the early warning signs?
Osteoporosis often progresses without symptoms or pain until a bone fracture occurs. A large number of patients remain unaware of their condition, and are therefore untreated — which is why early identification is crucial to prevention.
Are there any health conditions or medications that can increase the risk of osteoporosis?
Certain medications such as steroids, or conditions like malabsorption (the inability to digest or absorb nutrients from food) can increase one's risk. Some diseases like diabetes can interfere with calcium absorption and lead to osteoporosis.
When should we get ourselves checked for osteoporosis?
You are at risk if you have a history of fragility fractures, preexisting medical conditions, or are taking medication linked to bone loss. Dr Tay suggests osteoporosis screening for women above 65 and men above 70, or earlier at 50 if you have risk factors. Early identification is key to fracture prevention. To diagnose for osteoporosis, your doctor will recommend a painless bone mineral density (BMD) scan.
Busting common misconceptionsMyth: I'm a man so I'm safe from osteoporosis. Truth: Men can also be affected by osteoporosis.
Myth: Osteoporosis only affects older people. I don't have to worry about it now. Truth: We accumulate bone as we grow until around our late 20s so it's important to take note of bone health early. In exceptional cases, osteoporosis may also affect younger people. When women transit into menopause, they lose bone at the rate of about 2% per year. For men, bone loss occurs later in their 70s. If you take care of your peak bone mass, it lowers your chances of reaching the osteoporotic range later in life.
Myth: I'll know when I start to have weak bones. Truth: You won't be able to feel your bones getting weaker. But some possible signs can be height loss, teeth loss, or loss of grip strength. If you want to be sure, the best way is to get tested for osteoporosis by taking a bone mineral density (BMD) scan.
Myth: There is no cure or treatment for osteoporosis. Truth: While there is no cure for osteoporosis, there are effective treatments for osteoporosis that can help slow down bone loss and encourage new bone growth.
Myth: The risk of developing osteoporosis can't be reduced. Truth: Calcium, Vitamin D, and exercise can reduce the risk of osteoporosis. Calcium is an important building block for bones and Vitamin D helps your body absorb calcium. Exercise helps reduce the rate of bone loss and conserve bone tissue. |

The Road to Healthy Bones Starts with CDE
Include plenty of calcium in your diet
Calcium helps your muscles, blood vessels, nerves and cells work normally. If you don't get enough calcium, your body will take it out from your bones to keep your blood calcium level normal.
If you have a dairy-free diet
If you can't take dairy because of lactose intolerance or dietary preferences, look for calcium-fortified products and soy products with labels like "high calcium" or 'calcium fortified". You can also take yoghurt or hard cheeses as these have lower lactose content compared to fresh milk.
Pay attention to Vitamin D
Our digestive symptom does not absorb calcium well, so Vitamin D helps the gut absorb more calcium. It also regulates bone renewal and development. Foods like salmon, egg and cheese contain Vitamin D but are low in quantity. The best source is still direct exposure to sunlight. Get at least 15 minutes of sunlight a day to stimulate Vitamin D production in your skin.
Prioritise natural foods over supplements
Natural calcium-rich foods are preferred over supplements as they provide a variety of nutrients such as protein and vitamin B12 which you won't get from calcium supplements alone. Misuse of supplements may result in excessive intake of calcium or vitamin D (more than 4,000 international units per day) which could lead to health problems such as kidney stones and calcium deposits.
Drink less alcohol
Chronic heavy drinking increases the risk of osteoporosis by killing osteoblasts, the bone-building cells. Keep to one alcoholic drink for females and two for males daily. A standard drink = 330ml of beer, or 100ml wine, or 30ml hard liquor.
Exercise: Quality better than quantity
Do a combination of the recommended exercises below to reap their benefits. They work all major muscle groups including the legs, hips, back, abdomen, chest, arms and shoulders. Remember, quality of movement is more important than quantity - doing more repetitions may not always be better! See a physiotherapist for advice on the type of exercises that will be effective for you.

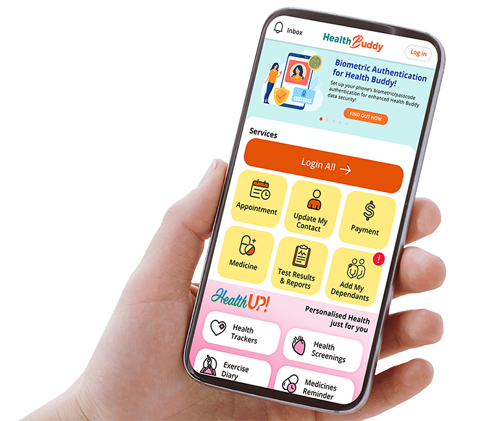
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.